Meibomian blepharitis
Definition
Generally speaking, dry eye conditions are a result of a lacrymal film disorder, due to either insufficient tear production or excessive evaporation of tears:
There are therefore two distinct and non-exclusive pathophysiological forms of dry eye syndrome:
1. The aqua-deficient form (insufficient secretion of tears)
Eye dryness through aqueous deficiency occurs when the principal or accessory lacrimal glands are altered and unable to moisten the eye.
2. The evaporative form (excessive evaporation of tears)
It is recognised that a large majority of cases are of the evaporative form, mainly caused by the absence or insufficiency of the external lipid layer of lacrymal film secreted by the meibomian glands.
Evaporative dry eye occurs when meibomian glands are defective, when the ocular surface is irregular, when the eyelid structure is abnormal or when contact lenses are worn, for example. Meibomian blepharitis belongs to the evaporative form of dry eye and is related to blockage of the meibomian glands (or tarsal glands). These glands, located in the lower and upper eyelids, are responsible for the production of the lipid layer of the tear film. When the glands are blocked, the lipid layer becomes insufficient in preventing evaporation of the tear film and providing lubrication of the surface.
The “evaporative” form of this condition accounts for 65% to 86% of patients affected by dry eyes. E-Eye is intended for patients suffering from the evaporative form of meibomian blepharitis.
Aims of the study
To demonstrate the effects of intense pulsed light in the treatment of meibomian gland dysfunction and to evaluate the safety and effectiveness of a pulsed light device in the treatment of MGD linked to meibomian blepharitis. These studies are based on different data: analysis of medical reports, testing of E-Eye, a clinical study of E-Eye in Australia and New Zealand, and another clinical study in China.
Study no 1
Treatment with a polychromatic pulsed light device for a dysfunction described as “dry eye” in the form of a corneal condition associated with a deficiency in the lipid layer, Dr Christian Malbrel, Ophthalmologist.
Study no. 2
Prospective trial of intense pulsed light for the treatment of meibomian gland dysfunction. Jennifer P. Craig, Yen-Heng Chen, et Philip R. K. Turnbull, Ocular Surface Laboratory, Department of Ophthalmology, New Zealand National Eye Centre, University of Auckland, Auckland, New Zealand.
Purpose
To evaluate the effect of intense pulsed light (IPL) applied to the periocular area in the treatment of meibomian gland dysfunction (MGD) via a prospective, double-masked, placebo-controlled, paired-eye study.
Methodology
Twenty-eight participants underwent IPL treatment (E-Eye, E-Swin, France), with homogeneously sequenced light pulses delivered to the periocular area of one eye and placebo treatment to the partner control eye at 1, 15, and 45 days following baseline (BL) evaluation. Lipid layer grade (LLG), non-invasive tear break-up time (NIBUT), tear evaporation rate (TER), tear meniscus height (TMH) and subjective symptom score using visual analogue scales (VAS) were compared with BL and control values at each visit.
Results
Lipid layer grade improved significantly from BL to Day (D) 45 in the treated eye (P< 0.001) but not the control eye (P = 0.714), with 82% of treated eyes improving by at least one LLG. Non-invasive tear break-up time also improved significantly from BL to D45 in the treated eye (P < 0.001) but not in the control eye (P = 0.056); it was significantly longer in the treated eye at D45 (14.1 ± 9.8 seconds versus 8.6 ± 8.2 seconds, P < 0.001). The tear evaporation rate was not different in the treated eye compared with the control eye at any visit. Tear meniscus height did not change from BL in either eye (P > 0.05). Visual analogue scale symptom scores improved from BL in the treated eye (P < 0.015), but not the control eye (P = 0.245), with 86% of participants noting reduced symptoms in the treated eye by D45.
Conclusion
Intense pulsed light with multiple sculpted pulses shows therapeutic potential for MGD, improving tear film quality and reducing symptoms of dry eye. (https://www.anzctr. org.au number, ACTRN12614000162617.)
This study was conducted with an E-Eye medical device, identical in all aspects (settings, physical characteristics) to E-Eye devices that are currently manufactured and marketed.
The person in charge of this study was Jennifer P. Craig, a qualified academic optometrist. Her main research interests include dry eye and tear film dysfunction, the cornea, contact lenses and refractive surgery. She currently heads the Ocular Surface Laboratory at the University of Auckland and regularly delivers continuing education and research lectures internationally, as well as publishing in both the scientific and clinical press. She conducted this study with Drs Turnbull and Chen. The clinical trial has been registered at ANZCTR (Australian New Zealand Clinical Trials Registry) under the request number 365741 and is available through this link: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=365741
Study no 3
Evaluation of the safety and effectiveness of the controlled discharge xenon flash lamp device in the treatment of dry eye caused by meibomian gland dysfunction, Dr Huibin Lv, Peking University Third Hospital Eye Center.
Purpose
Chronic inflammatory ocular surface dry eye, caused by meibomian gland dysfunction, is very common in clinic. The purpose of this study is to evaluate a new method – Controlled Discharge Xenon Flash Lamp Device – in the treatment of dry eye syndrome caused by meibomian gland dysfunction, its effectiveness and safety.
Equipment
An E-Eye machine was provided by E-Swin, France (www.e-swin.com).
Patients
Patients were enrolled into the study from July 2014 to October 2014, at the Third Hospital of Peking University. The criteria for enrollment and exclusion are shown in Table 1. For diagnosis, the dry eye syndrome should have lasted for at least 12 months, and the tear film break-up time (TBUT) should be less than 10s, while the meibomian gland orifice obstruction should be greater than or equal to grade 1. For the treatment group, all patients had 4 visits: first visit, then 2 weeks, 1 month and 2 months after the first visit. The Controlled Discharge Xenon Flash Lamp Device was applied to the patient at each visit (energy 13.0J/cm2).
Clinical evaluation
Clinical evaluation included: (1) assessment of dry eye syndrome, (2) eyelid (palpebral blunt, notch, vascular abnormalities, eyelash abnormalities, hyperkeratosis, front blepharitis), (3) meibomian gland (quantity at central 1cm, degree of obstruction, scar, deletion of orifice, nature of the secretion), (4) tear film (BUT, debris, tear foam, height of the upper and lower tear river), (5) cornea and conjunctiva (conjunctival hyperemia, conjunctival flabby, corneal staining).
Statistics
For evaluation of the symptoms, meibomian gland (central 1cm quantity, degree of obstruction, deletion, glandular secretion, tear film (BUT), debris, tear foam, height of upper and lower tear river), cornea and conjunctiva (conjunctival congestion, corneal staining, conjunctival relaxation), scores were analyzed using the paired test. For evaluation of eyelid (eyelid blunt, notch, vascular abnormalities, eyelash abnormalities, hyperkeratosis, front blepharitis) and meibomian gland (scar), the chi square test was used.
Results
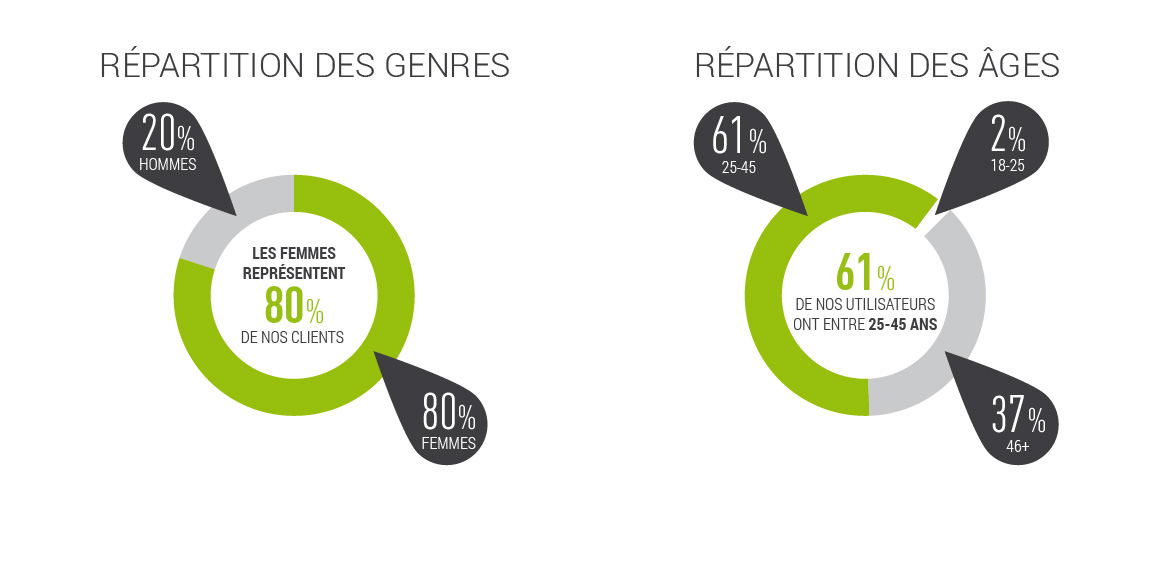
Demographic characteristics: The study evaluated 40 dry eye patients with 80 eyes, including 22 female patients (44 eyes) and 18 male patients (36 eyes). The mean age of patients was 51.3 + 20.1 years old (range 21-78 years old).
Conclusion
Using Controlled Discharge Xenon Flash Lamp Device treatment (energy level: 13.0J/cm2), the dry eye symptoms were significantly relieved in patients suffering with meibomian gland dysfunction caused dry eye, and the morphology of the palpebral margin, meibomian gland opening obstruction and meibomian gland quantity were also improved. All the differences between prior and post treatment were statistically significant. In addition, the Controlled Discharge Xenon Flash Lamp Device therapy was shown to improve the tear film quality and prolong the tear break-up time. Following 4 consecutive treatments, the improvement to the dry eye symptoms and the sign of the ocular tissues could be easily maintained. Overall, this study demonstrated that Controlled Discharge Xenon Flash Lamp Device treatment is safe and effective in the treatment of dry eye caused by meibomian gland dysfunction.
The effectiveness of Controlled Discharge Xenon Flash Lamp Device treatment was statistically significant for all the symptoms except blurred vision, while the improvement trends were similar to other signs. In this analysis, 13 symptoms were selected; each of them was scaled from 0 to 10 with 0 meaning no symptom and 10 meaning very serious. During each visit, the patient was asked to self-evaluate the 13 symptoms, and all the evaluations were documented.